The Mpox virus has plagued Africa for decades, but the recent outbreak has highlighted a stark and troubling reality: Africa is once again left behind in the global race for vaccines. As the virus continues to wreak havoc, especially in countries like the Democratic Republic of Congo (DRC), the delay in vaccine distribution has exposed a significant gap in global health equity. This article delves into the complex web of bureaucracy, the challenges of vaccine distribution in low-income countries, and the urgent need for a more streamlined approach to global health emergencies.
The Unfolding Crisis: Mpox in the Democratic Republic of Congo
Given the deeply rooted virus in the region, the Congo was a traditionally natural haven for Mpox outbreaks. In 2024, things went to another dimension: more than 27,000 suspected cases, with 1,100 deaths, mainly among children. The Clade 1 Mpox virus is considered one of the most lethal types of the virus, and that has been behind this appalling crisis that is rapidly spreading across eastern Congo into other neighboring countries.
Even with the outbreak’s intensity, the Democratic Republic of the Congo and other African countries have had difficulty getting immunizations. On August 14, 2024, the World Health Organization (WHO) proclaimed a worldwide health emergency; yet, the reaction to this disaster has been startlingly delayed. The effectiveness of the global health system in handling emergencies in low-income nations has come under scrutiny due to this delay.
WHO’s Regulatory Process and Its Impact
The World Health Organization (WHO) plays a crucial role in vaccine distribution, especially for low-income countries. However, their regulatory process has caused delays in getting vaccines to people who urgently need them. The WHO has a procedure called vaccine prequalification. This is an important step that must be completed before vaccines can be given out in poorer nations. Unfortunately, this process has been moving very slowly.
Many people have criticized the WHO for being too careful and focused on following rules, instead of taking quick action during emergencies. They say the organization is more concerned with avoiding risks than with getting vaccines to people quickly.
These delays at the WHO have become a major problem in the effort to distribute vaccines worldwide. The slow regulatory process is preventing vaccines from reaching those who need them most, especially in countries with less money and resources. Read More- https://ecoti.in/_LGf8Z
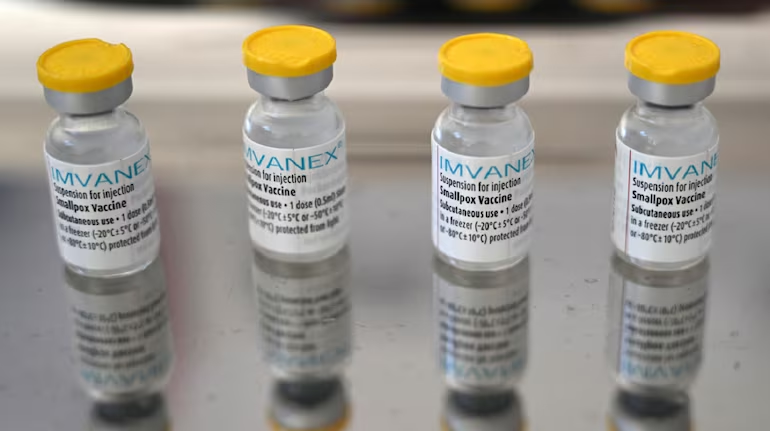
The Jynneos vaccine, produced by Bavarian Nordic, and the LC16 vaccine from Japan’s KM Biologics, have both been delayed by this regulatory process. During the 2022 Mpox outbreak, the vaccine was widely used in North America and Europe to help control the spread of the virus. However, the World Health Organization (WHO) did not start its formal review process for the Jynneos vaccine until mid-2024. This is a significant delay compared to its use in other regions.
Because of this delay, African nations have lacked an important tool to fight against Mpox effectively. This situation highlights how delays in the WHO’s approval process can have real-world impacts on public health, especially in regions that rely on WHO guidance for vaccine use.
Content Highlights:
- Africa’s severe Mpox outbreak and the urgent need for vaccines.
- WHO’s delayed vaccine approval process and its impact on African nations.
- The growing disparity in global health responses between high-income and low-income countries.
- Concerns over the effective deployment of vaccines, especially for vulnerable children.
- The ongoing debate about WHO’s role in hindering or helping during health crises in Africa.
The Complexities of Vaccine Deployment in Africa
Even when vaccinations continue to reach Africa, deployment obstacles remain staggering. Health clinics in Congo and other nations are unable to store the Jynneos vaccine at below 20 degrees Celsius. Furthermore, while the LC16 vaccine is safe for children, it requires a specialized needle for injection, preventing its availability.
Public health officials in Africa are facing a daunting challenge as they attempt to control the rapidly spreading Mpox outbreak. The arrival of 10,000 doses of the Jynneos vaccine, donated by the United States, offers a glimmer of hope. However, this limited supply falls far short of meeting the actual need on the ground.
With the virus now present in 13 African countries and showing no signs of slowing down, health authorities are forced to make difficult decisions about vaccine prioritization. The question looms large: Who should receive these scarce doses first? The situation is further complicated by the need for a vaccination strategy that can be quickly scaled up as more supplies become available. Officials must balance immediate needs with long-term planning, all while racing against the clock to prevent further spread of the virus.
A Call for Global Solidarity
The ongoing Mpox crisis has exposed serious flaws in the global health emergency response system. This situation calls for major changes in how the world handles such crises: The World Health Organization (WHO), Gavi, and other international health organizations must enhance their procedures. They need to figure out how to accelerate and simplify their regulatory processes without sacrificing vaccination safety.
As much time as possible should be spent getting immunizations to those who require them. Lives are being endangered by the present sluggish distribution and approval process. Also read : https://theaspectratio.in/health-fitness/from-congo-to-the-world-whos-emergency-meeting-on-monkeypox-could-change-everything/
High-income countries need to very seriously increase support to access to vaccines in poorer regions. This is beyond the donation of vaccines—although that itself is important. The solution should be to take a more advanced look at deeper inequalities that worsen these crises in low-income countries from these wealthy nations themselves. This would either mean building better healthcare systems or supporting local vaccine production.
The outbreak of Mpox is very illustrative that the current way of doing things simply does not work well enough, leaving people in vulnerable populations without appropriate protection for too long.
Only through global solidarity, equitable access to vaccines, and a more agile response to health emergencies can we hope to prevent future crises and protect the most vulnerable populations.



 By
By